Shift work sleep disorder (SWSD) is not just “being tired after a night shift.” It is a recognized circadian rhythm disorder that affects millions of people whose jobs require overnight, rotating, or early-morning schedules. Nurses, factory workers, emergency responders, pilots, and IT professionals often experience persistent insomnia, excessive sleepiness, or both.
Over time, this misalignment between biological time and social time erodes health, cognition, and mood. In clinical settings, physicians often observe that patients with SWSD feel dismissed or blamed for “poor sleep hygiene,” even when they are doing everything right. Fixing shift work sleep disorder requires understanding biology first—and willpower second.
Definitions & mechanisms — what actually goes wrong
Shift work sleep disorder occurs when the circadian rhythm—the brain’s internal 24-hour clock—cannot adapt to externally imposed work hours. The master clock in the hypothalamus is synchronized primarily by light exposure, not by motivation or habit.
When a person works nights and sleeps during the day, light signals conflict with melatonin release, cortisol rhythms, and core body temperature cycles. The result is fragmented sleep, reduced REM duration, and impaired alertness during work hours.
Neurochemically, wakefulness is regulated by histamine, dopamine, norepinephrine, and orexin systems. Many wake-promoting agents target these pathways, which is why eugeroics have a distinct role compared with classic stimulants.
A structured overview of these agents can be found in the Eugeroic drug list, which categorizes wake-promoting medications by mechanism and clinical use.
Why lifestyle advice alone often fails
Standard advice—“sleep in a dark room,” “avoid caffeine,” “keep a schedule”—is necessary but frequently insufficient for true SWSD. The core problem is not behavior; it is forced circadian misalignment.
Many patients report that even after years on the same night shift, their bodies never fully adjust. This is consistent with research showing that only a minority of adults can permanently invert their circadian rhythm without physiological cost.
This explains why off-label pharmacological strategies are often explored, not as shortcuts, but as compensatory tools when biology resists adaptation.
Clinical insights — what physicians actually see
Sleep specialists often distinguish between temporary shift-related insomnia and chronic SWSD. The latter is marked by symptoms persisting for at least three months, despite adequate opportunity for sleep.
Clinically, doctors observe:
- Increased workplace errors and near-miss accidents
- Higher rates of depression and anxiety
- Metabolic changes, including insulin resistance
- Cardiovascular strain over long-term exposure
Importantly, many patients underreport symptoms until performance or safety becomes an issue. Early intervention is associated with better outcomes.
Consulting a qualified Doctor—particularly one trained in sleep medicine—can help differentiate SWSD from primary insomnia or sleep apnea.
Evidence-based strategies to fix shift work sleep disorder
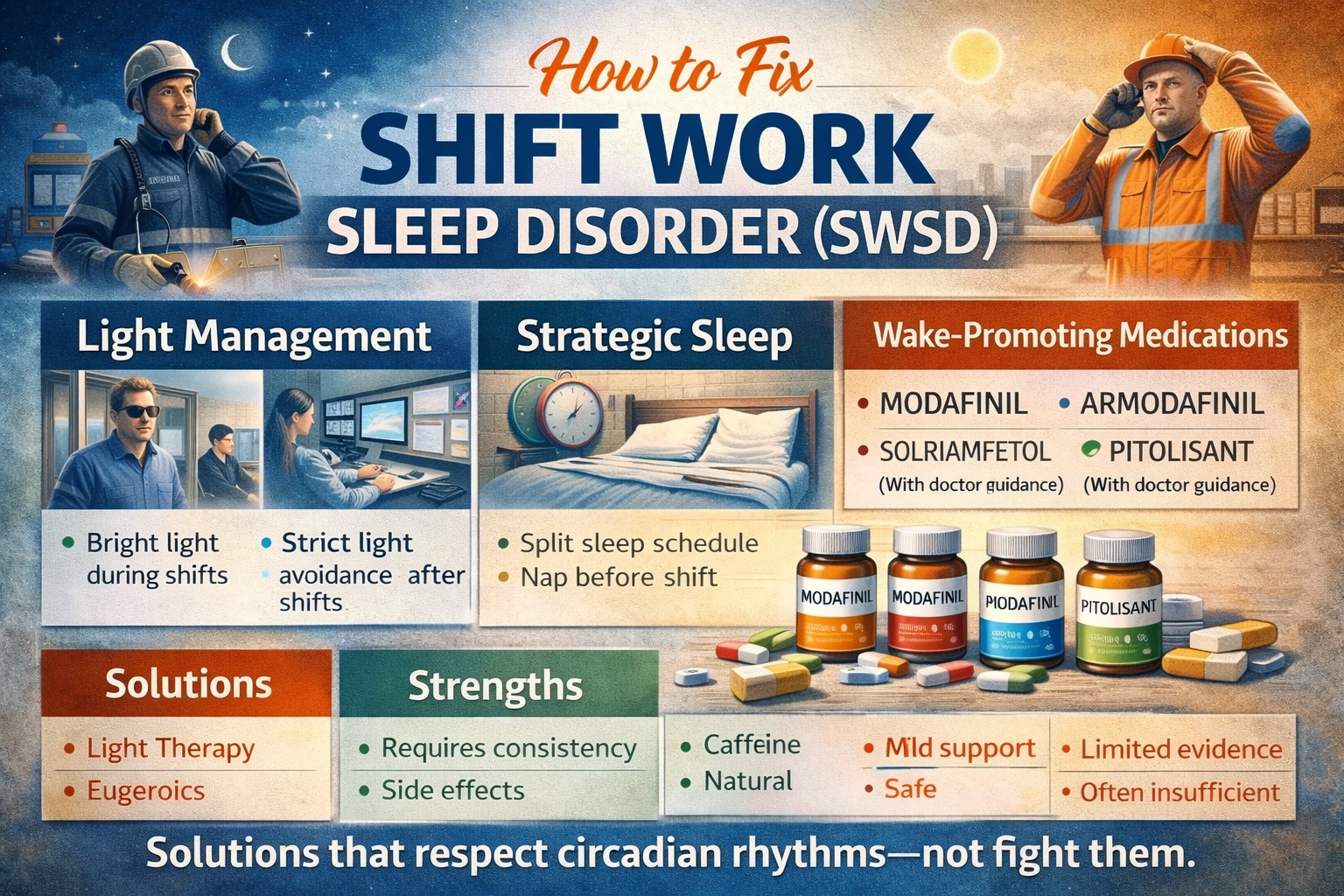
A. Light management (the cornerstone)
Timed light exposure is the most powerful non-drug intervention. Bright light during night shifts (especially early in the shift) suppresses melatonin and improves alertness. Conversely, strict light avoidance after work—using sunglasses and blackout curtains—protects daytime sleep.
B. Strategic sleep scheduling
Rather than trying to sleep eight continuous hours, many clinicians recommend split sleep: a core sleep period plus a shorter nap before work. This aligns better with circadian biology for some individuals.
C. Caffeine, used precisely
Caffeine can help, but timing matters. Consumed too late, it worsens post-shift sleep. Used early in the shift, it may support alertness without disrupting recovery.
Pharmacological options — where eugeroics fit
Wake-promoting agents
For moderate to severe SWSD, clinicians may consider wake-promoting medications. These differ fundamentally from amphetamines.
- Modafinil is FDA-approved for shift work sleep disorder in the U.S. It enhances alertness primarily through dopaminergic and orexin-related pathways, without the sharp peaks of classic stimulants.
- Armodafinil, its longer-acting enantiomer, may offer more sustained coverage for extended shifts.
- Solriamfetol acts on dopamine and norepinephrine reuptake and is often described as more energizing but less subtle.
- Pitolisant works via histamine H3 receptor antagonism and may feel cognitively “lighter” for some users.
Risks & side effects — the trade-offs
No pharmacological solution is risk-free. Common Side effects reported with eugeroics include headache, nausea, appetite suppression, anxiety, and insomnia if mistimed.
Physicians caution against combining eugeroics with Stimulants such as amphetamines, which increases cardiovascular and psychiatric risk. Comparisons with Adderall often highlight fewer emotional swings but also less motivational drive.
Long-term safety data in healthy shift workers remains limited. Medication should be viewed as part of a broader strategy, not a standalone fix.
Use cases, comparisons & alternatives
| Approach | Strengths | Limitations |
|---|---|---|
| Light therapy | Non-pharmacological, effective | Requires consistency |
| Eugeroics | Improve alertness, FDA-backed | Timing-sensitive, side effects |
| Natural eugeroics | Mild support | Limited evidence |
| OTC eugeroics | Accessible | Variable quality |
| Lifestyle-only | Safe | Often insufficient |
Some workers explore compounds Like eugeroics or performance strategies adapted from Sports science, such as circadian training and recovery planning.
Ultimately, the Best eugeroic is highly individual and depends on shift length, health history, and tolerance.
Regulatory notes & sourcing considerations
In the United States, modafinil and armodafinil are prescription-only and regulated by the FDA. The FDA’s drug safety communications outline approved indications and risks for wake-promoting agents:
The National Institutes of Health provide neutral summaries on circadian rhythm disorders and sleep health:
- NIH: https://www.nih.gov
Workers should be cautious when researching Modafinil vendors, as legality, quality control, and counterfeit risk vary.
Conclusion — fixing SWSD is about alignment, not willpower
Shift work sleep disorder is a physiological mismatch, not a personal failure. The most effective solutions combine light management, strategic sleep, and—when appropriate—carefully chosen pharmacological support.
Eugeroics can help people Get work done safely during biologically adverse hours, but they do not replace sleep or erase long-term risks. Sustainable improvement comes from respecting circadian biology, not fighting it.
External authoritative citations
- U.S. Food and Drug Administration (FDA): https://www.fda.gov/drugs
- National Institutes of Health (NIH): https://www.nih.gov